Hypospadias Re-Do Surgery – Pediatric
Home > Hypospadias > Hypospadias Re-Do Surgery – Pediatric
We often manage patients who have had repairs that have failed. Sometimes the urethral openings are still not placed correctly, and there is also not enough skin to use in the reconstruction of the urethral opening. This condition requires a complex approach that may include the use of skin grafts from other parts of the body. Although these repairs are more involved, and may require a staged approach, a successful outcome is often achieved.

Adequate Penile skin

Urethral opening at the tip of the penis
The urethral imaging, unfortunately, revealed that there was a stricture of the entire previously reconstructed urethra extending from the tip of the penis to the portion of the urethra next to the prostate under the scrotum.
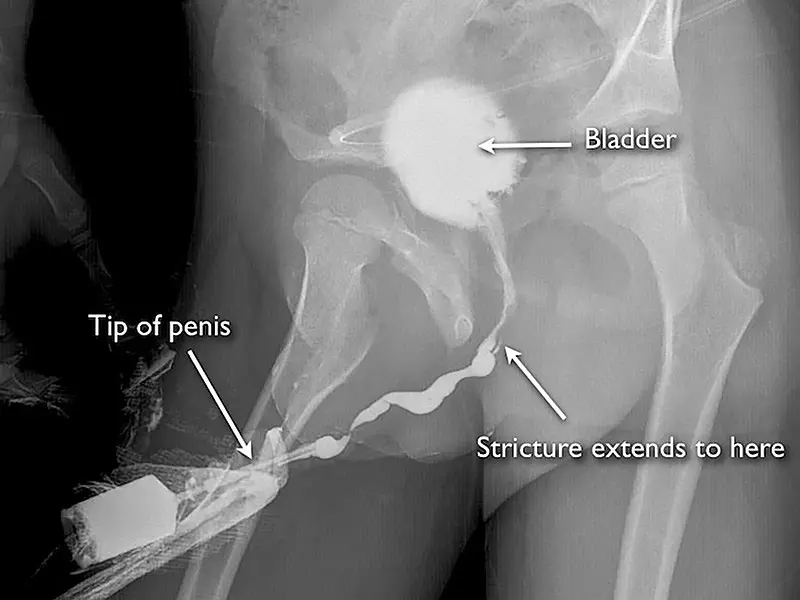
Retrograde urethrogram demonstrating severe pan-urethral stricture disease after prior hypospadias surgery
This problem is best managed with a staged urethral reconstruction using buccal mucosa grafts (tissue from inside of the cheek) and split-thickness skin grafts from the thigh.

Undersurface of the penis

Severe penile skin deficiency
This patient did not have any significant penile length with erections and was sexually disabled. In these cases, the priority is to treat any urethral stricture disease and skin graft the penis (split thickness graft) so that sexual intercourse will be possible. At the conclusion of the surgery, there is no urethral obstruction and the penis will have adequate length for intercourse. However, the urethral opening will not be at the tip of the penis. Options at that point include staged urethral reconstruction or maintaining the urethral opening at the undersurface of the penis. In this case, we were able to subsequently reconstruct the urethra to bring the urethral opening along the distal shaft of the penis, but it was not practical to bring the opening to the tip of the penis. Staged urethral reconstruction after penile skin grafting is very problematic as the blood supply to the tissues is marginal. In these challenging cases, we can not always achieve a perfect cosmetic and functional result. However, we can generally create a situation where the patient can be sexually active and urinate without obstruction and have an improved cosmetic appearance of the penis.