After a complete diagnostic evaluation is made, we begin BXO treatment. The approach to this condition should be individualized, as one’s BXO treatment plan varies based on one’s symptoms and the findings of the testing. A comprehensive plan is best formulated by a urologist with expertise in male urethral and penile disorders. While some of the skin changes respond favorably to topical steroid cream (such as Temovate 0.05%), no topical cream can provide a cure for any associated strictures.
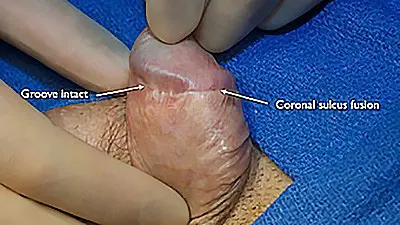
In some specific cases, circumcision may be beneficial; however, circumcision is only helpful in select cases where there is redundant diseased skin. Most of the time, circumcision in a circumcised patient could lead to a skin deficiency. If there is adequate skin length, but there is a narrowing and pinching the distal skin towards the head of the penis, Dr. Gelman can try an innovative BXO treatment that consists of making longitudinal incisions and transverse closures along the penile skin. This revision surgery adds width where needed without having to remove any skin.
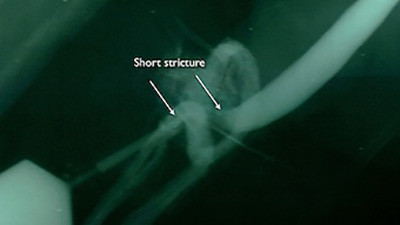
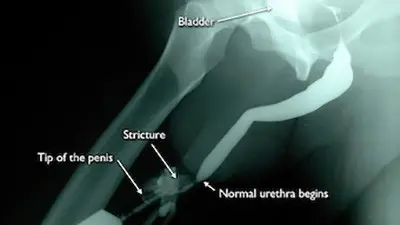
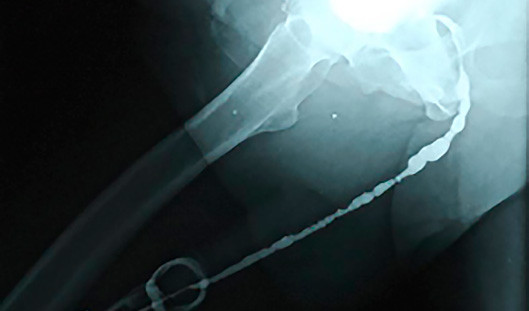
When BXO is associated with urethral stricture disease, it is best to avoid observation or dilation to treat the stricture. The best treatment depends on the length of the stricture. The ideal treatment for the management of very short strictures is a meatotomy or extended meatotomy, which is a simple effective procedure to cut open the narrow opening in the operating room. For longer strictures, the recommended treatment is a urethroplasty (open urethral reconstruction).
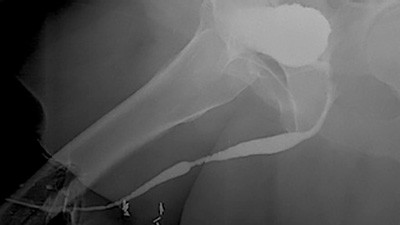
The most complex strictures associated with BXO are pan-urethral strictures, which involve the entire anterior urethra and can measure over 22 cm in length. Although these are incredibly complex strictures that can prove quite difficult to treat, the Center for Reconstructive Urology has successfully reconstructed the urethra of many patients with this problem over the past 21 years.
In the past, it was reported that using penile skin as a tissue to augment the narrow urethra could lead to a high rate of BXO recurrence. It was suggested that because the disease involves penile skin, the recurrence may be due to the disease progressing into the penile skin. It was proposed that if distant tissues (buccal mucosa tissue from inside the cheek or extra-genital skin grafts from the thigh) were used instead of penile skin, perhaps the long-term success rate would improve.
Our preferred approach for many years was to reconstruct the bulbar urethra (the urethra under the penis) in one-stage using bilateral buccal mucosa grafts. For the remainder of the urethra, we typically used to perform a first repair using a split-thickness skin graft taken from the thigh. During the first stage, the skin graft was placed adjacent to the urethra, and, following surgery, the opening of the urethra was at the base of the penis. Over the next 4-6+ months, the graft became more supple and could be rolled into a tube to reconstruct the urethra, setting the stage for the second step of repair.
What we noticed was that our technical success rate (at 4 month check) was 100% for our patients. Also, when only tissue from inside the cheek was used, the long term success rate has been 100% so far. However, when any thigh skin grafts were used, although out technical short term results were 100% success, there were late failures indicating that thigh grafts do not hold up as well as we would like. We presented our findings at the 2019 meeting of the American Urological Association and hope to publish this data this year.
Although our technical success rate with BXO treatment is very high, there will always be a risk of late recurrence with this disease. While surgery addresses the obstruction, it is not by any means a BXO cure. Therefore, life–long follow-up is incredibly important for any patient diagnosed with Lichen Sclerosis.