Diagnostic Evaluation
Home > Prostate Cancer Complications > Diagnostic Evaluation
Diagnostic Evaluation: Prostate Surgery, Radiation, and HIFU Side Effects
Prior to any treatment, a complete evaluation of the bladder and the urethra is important. The following is an illustration of the anatomy of the male urethra.
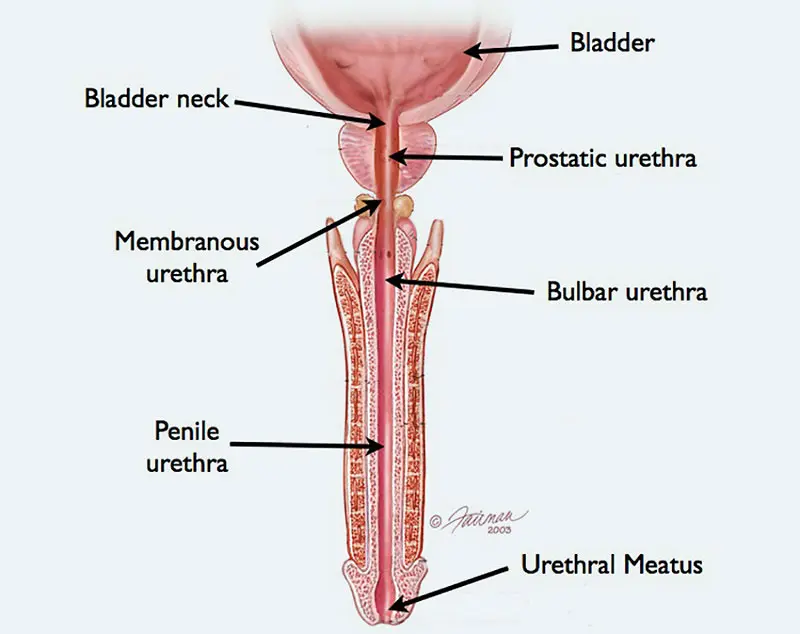
The connection of the prostate to the bladder is called the bladder neck. This is a main area of continence. The bladder neck is normally closed except during urination, when the bladder neck opens as the bladder squeezes (contracts) to empty. The prostatic urethra is the portion of the urethra that travels through the prostate itself. On the other side of the prostate is a short segment of urethra called the membranous urethra, and this is surrounded by a muscle called the external sphincter. This area of the urethra is also pinched closed except during urination. The bladder neck and external sphincter are the 2 main continence mechanisms that prevent the involuntary leakage of urine (incontinence). The remaining urethra between the membranous urethra (from the bulbar urethra to the tip of the penis) is a tube that is not related to continence. This is called the anterior urethra.
When men develop urethral strictures unrelated to prostate cancer treatment, the stricture is not at or near the level of the prostate. Incontinence is not a concern, and the stricture can be reached during open repair without difficulty through an incision under the scrotum (called a perineal approach) or through a circumcising penile skin incision. When men have strictures away from the area of the bladder and prostate, narrowing of the urethra is the only problem, and this can be repaired at our Center with an extremely high success rate, even when the strictures are long and/or recurrent. One type of anterior stricture that men can develop after prostate cancer treatment related to the placement of instruments or catheters through the urethra is a stricture limited to the urethra just deep to the urethral opening at the time of the penis. This called a fossa navicularis stricture and is highly amenable to definitive repair.
In contrast, blockage adjacent to the prostate is a different and more complicated problem. After the prostate has been removed, continence is mainly provided by the external sphincter, an area that can be damaged during prostatectomy. When there is a narrowing of the area where the bladder is attached to the urethra after prostate removal, this is called a bladder neck contracture. Unlike urethral strictures, bladder neck contractures are not easily reached through an incision under the scrotum or through the lower abdomen. The bladder neck is deep within the pelvis and hard to reach. Moreover, patients with bladder neck contractures may also have incontinence whereas this is not an issue when there is an anterior urethral stricture.
After radiation or high frequency focused ultrasound (HIFU), if there is a stricture limited to the area of the membranous urethra, then this can be repaired with open excision of the scar and re-anastomosis (cutting out the bad part and putting the 2 healthy ends back together. However, the bladder neck must also be free of blockage because it is not beneficial to treat one area of blockage if there is another cause of obstruction. In addition, if the bladder neck does not remain closed except during urination, the treatment of a membranous stricture may be associated with the development of incontinence. In addition, radiation and HIFU can damage the bladder, decreasing the capacity significantly. In these cases, addressing only the urethral problem will not lead to normal urination. For the above reasons, it is important to assess all areas of the urethra and the bladder neck for the presence or absence of stricture, define the exact length and location of any stricture, assess the continence mechanisms, and the bladder capacity and function.
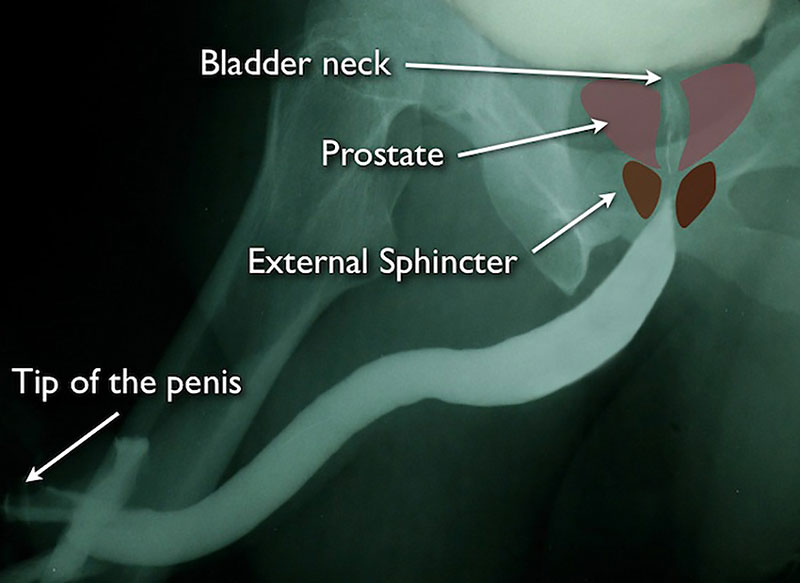
Graphics of the external sphincter and prostate superimposed on a normal retrograde urethrogram (RUG). Notice that the membranous urethra (surrounded by the external sphincter) and bladder neck are both closed. The patient is not urinating during this study and it is normal for these areas of be pinched closed.
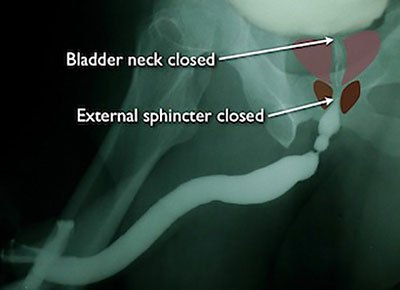
This is the retrograde urethrogram (RUG) in a patient with a bulbar urethral stricture away from the prostate. Notice that the bladder neck and external sphincters are closed. This is normal.
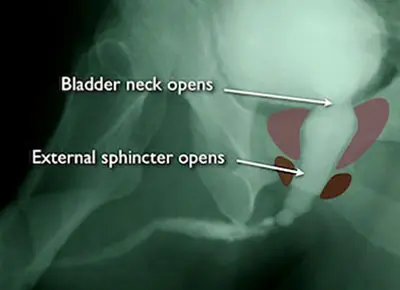
This film was taken when the same patient urinated (the study is called a voiding cystourethrogram, or VCUG). Notice that the bladder neck or external sphincters are wide open.
We perform complete imaging that includes both a RUG and VCUG. Since the bladder neck and external shincter areas are closed when a patient is not urinating and open during urination, the VCUG (taken during urination) is the best imaging study to evaluate the bladder neck and membranous urethra (external sphincter area). Urethral imaging also identifies any rectal-urethral fistula, an abnormal communicatioin between the urethra and rectum as during injection, contrast fills the rectum.