Hypospadias Diagnostic Evaluation
Home > Hypospadias > Hypospadias Diagnostic Evaluation
Opening under the head of the penis in a patient with a urethral stricture after hypspadias repair (elsewhere).

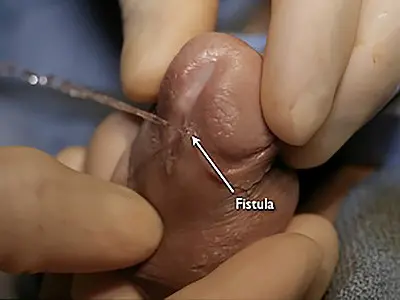
Fistula, an opening to the side of the distal penis after prior failed hypospadias surgery.
Infants and young children born with hypospadias often undergo hypospadias treatment with surgical repair without any testing to evaluate the urethra as urethral stricture disease is not generally present. However, untreated hypospadias is a risk factor for the development of urethral stricture disease in adults. Therefore, when adults present to the Center for Reconstructive Urology requesting hypospadias repair, we calibrate the urethral opening using instruments called Bougies. Although these instruments are long, the time is advanced only for a very short distance (less than 1 inch) and then removed. We start with the smallest instrument (9 French which is only approximately 3 mm diameter) and use lidocaine jelly. If there is any resistance to the advancement or withdrawal of the instrument, we know that the opening is no greater than 9 French. Therefore, we do not attempt to pass any larger instruments as this would then dilate the urethra and cause discomfort. Our objective is not to dilate the urethra, but rather painlessly determine if the urethra at and near the opening is normal in size or narrow. If the 9 French bougie advances and withdraws easily, we then use the next larger size, and continue with larger instruments until there is very slight resistance during insertion or withdrawal. At that point, the size of the distal (towards the tip) urethra is known.

Single bougie close up

Bougie set
We then perform urethroscopy, a test involving the gentle advancement of a small telescope through the urethra to assess the caliber (size) of the urethra. Often, we use a pediatric scope even in adults as these smaller instruments advance though strictures. We never try to force our way though a stricture. If an area of the urethra is encountered that is smaller than the scope, we then immediately withdraw the scope. We do not use the scope as a dilation tool. In children, testing to evaluate the urethra may need to be performed in the operating room. Although these tests are not painful, children often will not tolerate procedures in the office setting, and we never want our patients to have unpleasant experiences.
When children or adults are referred for re-do repair after failed hypospadias surgery, a complete evaluation is necessary. If calibration and/or urethroscopy reveal a urethral stricture, a retrograde urethrogram (RUG) and cystourethrogram is performed (VCUG) to assess the exact length, location, ad severity of the urethral stricture. Details of the technique of proper and complete urethral imaging can be found in the diagnostic evaluation sub-section of the urethral stricture section.
The following patient was born with hypospadias. He underwent multiple failed repairs at a Children’s hospital complicated by urethral stricture disease. Urethral imaging that was obtained prior to referral suggested a short stricture according to the report and the arrows drawn on the film. However, the technique was poor, and repeat imaging confirmed a stricture extending from the opening of the urethra extending along the entire anterior urethra toward the sphincter (the area near the prostate deep to the scrotum) as shown. It is important to know the exact length, location, and severity of any urethral stricture disease prior to surgical treatment. Although one approach is to assess the urethra as the surgery is being performed, we prefer to obtain this information prior to surgery as this influences our approach.

Outside flouroscopy image suggesting short stricture
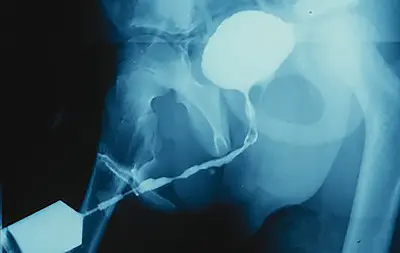
Repeat imaging showing stricture of the entire anterior urethra