Urethral Stricture Diagnostic Evaluation
Home > Urethral Stricture > Urethral Stricture Diagnostic Evaluation
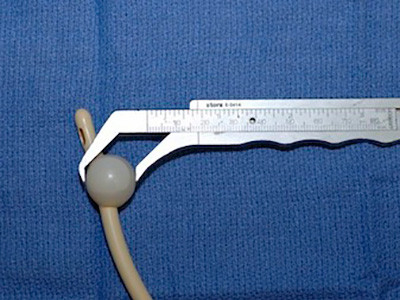
Bougie Calibration
When the opening of the urethra at the tip of the penis (urethral meatus) is narrow or if there is narrowing just deep to the urethral opening (an area called the “fossa navicularis”), the best way to determine the actual caliber (circumference = size) of the urethra of this portion of the urethra is with instruments called Bougie-a-boules.

Set of Bougie-a-Boules

Bougie being used
These cone shaped instruments painlessly measure the circumference of the opening of the urethra the way feeler gauges precisely measure the gap on a spark plug. The measurement of the caliber of the urethra is in French size. French is a measurement of millimeters circumference, and the French size is generally 3 times the diameter. Simply put, the goal is to evaluate the urethra at the tip of the penis to see if there is urethral stenosis there, or if the stricture starts further inside the urethra. A normal adult urethra is greater than 30mm circumference (30 French, approximately 10mm or 1cm diameter) except in the area near the tip of the penis, where the opening is normally approximately 24 French.
When we calibrate the distal (the part closest to the tip) urethra is calibrated, numbing lubricant is placed at the opening of the urethra, and a very small bougie, generally 8 French, is advanced a short distance and then removed. Unless the distal urethra is less than 8 French, the instrument will pass without any resistance. A 9.5 French Bougie is then advanced. We continue the procedure with larger instruments until there is a slight resistance, generally felt as the instrument is removed given that bougies are cone shaped. Once there is very slight resistance, this is the caliber of the urethra. No further instruments are placed as to continue with larger instruments would only dilate/tear the urethra causing pain, and our objective is to painlessly measure the size of the opening. In looking at the pictures of these long metal instruments, one may think the procedure involves jamming these through the penis. However, that is not how they are used (at least at our Center). The instrument is generally advanced only 1 inch after numbing jelly lubricant is placed.
Male Cystoscopy – Urethroscopy
Another part of the diagnostic evaluation for a urethral stricture is a urethroscopy. A urethroscopy is a procedure performed in the office setting. After gently instilling lubricant into the tip of the penis that contains lidocaine, a small (16 French telescope is gently placed into the urethra with advancement to the stricture. This instrument is called a cystoscope or a “penis scope”. It is a flexible tube that has an eye piece at one end and an opening at the opposite tip that allows light to shine through. The procedure is often called cystoscopy, but technically, if the penis scope is just advanced into the urethra and not all the way to the bladder, the procedure is called urethroscopy.
Flexible Scope
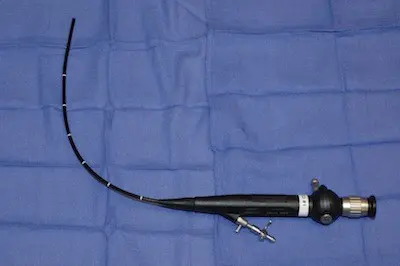
When male cystoscopy is performed, the gentle advancement of this instrument through the tip of the penis allows the Urologist to look inside of the urethra. It is our practice to use a digital cystoscope connected to a high definition monitor so our patients can see the inside of their urethra as the procedure is being performed. Often, the urethra is normal for some distance, and then a stricture is encountered. Once the stricture is smaller than the size of the scope, the cystoscope should be removed, and no attempt should be made to advance the scope through the stricture if the objective is to evaluate the urethra. Any forceful pushing to advance the scope through the area of disease towards the bladder will dilate and possibly tear the urethra.
When there is narrowing of the urethra near the tip of the penis that prevents the use of a 16 French scope, we use a 10 French pediatric cystoscope-urethroscope.
Pediatric Cystoscope

This is a smaller instrument than the flexible cystoscope and is 10mm circumference in size. The visualization is not as good when using this smaller instrument, but when the caliber of the distal urethra is between 10-16 French, the larger scope can’t be used. When the caliber of the urethra is smaller than the scope towards the tip of the penis (distal urethra), we do not attempt urethroscopy because we know that we cannot pass the instrument even a short distance.
Urethroscopy provides a direct look at the appearance along the length of the urethra up to the beginning of the stricture, and also a direct look at the stricture when the urethral stricture is first encountered. However, since the scope cannot be advanced through the stricture without trauma, the exact length of the stricture and the presence or absence of any additional strictures cannot be determined with urethroscopy using s cystoscopy-urethroscope. This highly important additional information is best obtained with X-ray contrast imaging called a retrograde urethrogram (RUG) and voiding cystourethrogram (VCUG).
Overview
The standard procedures for urethral imaging are a retrograde urethrogram (RUG) and a voiding cystourethrogram (VCUG). These are X-ray procedures that we perform in the office, often at the same time as cystoscopy. Films are taken during injection, and during voiding. These studies, when properly performed, will always define the exact location and length of the urethral stricture. It is essential to know this information prior to discussing urethral stricture treatment options, as the treatment decision should be based on first knowing all of the details related to the stricture, not just that there is one!.
Retrograde Urethrogram (RUG)
The retrograde urethrogram (RUG), which is in countries outside the USA also called an ascending urethrogram, is performed with the patient in the oblique position. This means that the patient is tilted 45 degrees. An initial film (called a scout film) is obtained before the actual procedure is performed. This is to confirm that the position and exposure is correct before any contrast is instilled. Then, gauze is gently wrapped around the head of the penis and gentle traction is applied to place the penis on stretch. This is painless. Then, contrast is gently instilled into the urethra using a specialized adaptor developed by Dr. Gelman.
This adaptor, called the Gelman Adaptor, is now commercially available. Dr. Gelman has no financial relationship with the medical device company for this or other inventions, and chose to avoid all industry relationships where there would be monetary compensation to avoid a conflict of interest. This adaptor is now pictured in the major textbook of Urology called Campbell-Walsh Urology.
The adaptor painlessly forms a seal at the tip of the penis. No needles or catheters are required and no balloons are ever inflated in the urethra.

Gauze in place

Contrast slowly instilled
As contrast (clear fluid that looks like water but appears bright white on an X-ray) is injected, a film is obtained. This study permits visualization of the entire urethra. This is an example of a RUG when the anterior urethra is normal.

The retrograde urethrogram, also called a RUG, best evaluates the anterior urethra. As previously mentioned, this is the portion of the urethra between the tip of the penis and the beginning of the posterior urethra (the membranous and prostatic urethra and bladder neck). Think about the anterior urethra as a tube or a hose that has nothing to do with leakage. The tube just transports urine. The RUG only provides very limited information about the posterior urethra, the part between the anterior urethra and the bladder. This is because the posterior urethra is not like a hose and has sphincters that open (during urination) and close (all other times). During the injection of contrast, the patient is not voiding, and when a patient is not voiding, the sphincters along the posterior urethra in the area near the prostate are closed, and the prostatic urethra is narrow. It is normal for the posterior urethra to be narrow and pinched off as a RUG is performed. If the external sphincter muscle and prostate were visible on the film, the image would appear as shown below.
Since the posterior urethra may be narrow because of a stricture, or may be narrow because it is normal, you can’t diagnose a stricture of the posterior urethra with a RUG. Therefore, while a RUG is the best imaging test to evaluate the anterior urethra, it is a poor study to evaluate the posterior urethra.
RUG with superimposed graphics demonstrating the prostate and external sphincter (red)
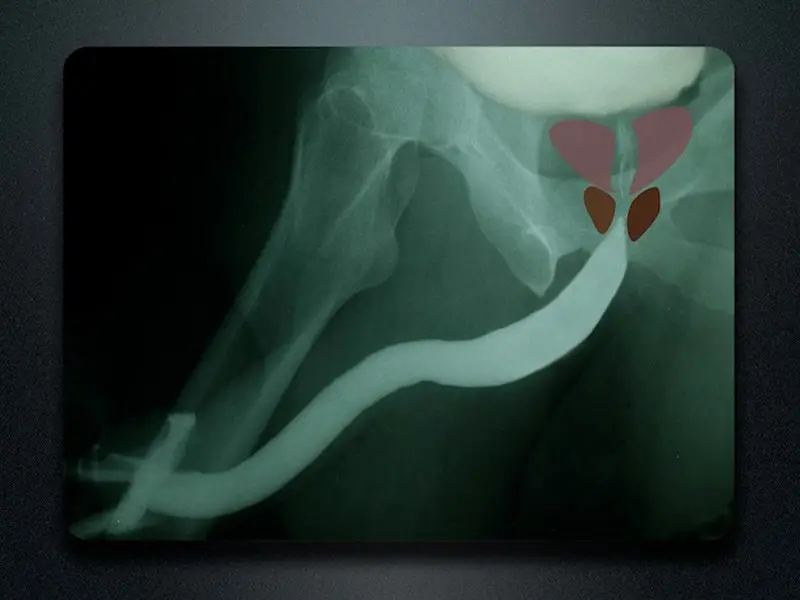
In a patient with a bulbar urethral stricture (bulbar is part of the anterior urethra), contrast passes through the stricture and outlines the area of narrowing and the normal area proximal to the stricture (proximal means on the bladder side of the stricture). Look at how narrow the urethra is at this point. However, since the patient was able to pass urine through the stricture, contrast could be instilled backwards to outline the urethra on both sides of the stricture. As long as there is some opening, since fluid can pass through small spaces, we are able to obtain excellent visualization of the entire urethra, something that can’t be done when only flexible cystoscopy is performed.
Film demonstrating bulbar stricture

Voiding Cystourethrogram (VCUG)
The VCUG is the best study to evaluate the posterior urethra. This is how it is done: As the RUG is performed, some contrast enters the bladder, and this can be seen on the film. The patient is then asked to urinate, and during urination, a film is obtained. It is often the case that patients are unable to void (urinate) after contrast is injected during the RUG as only 60cc of contrast (a small amount) is instilled for this study, and the patient simply may not feel the urge to urinate. Dr. Gelman will then instill additional contrast very, very slowly as to not cause pain until there is an urge for the patient to urinate. During urination, the bladder neck and external sphincters of the posterior urethra are supposed to relax and open as the bladder is contracting. It is a normal reflex. If the posterior urethra is widely patent during voiding, this confirms that this portion of the urethra is normal.
The following is a RUG and VCUG in a patient with a bulbar stricture. Graphics are superimposed (on the VCUG) to show the location of the prostate and external sphincter muscle (posterior urethra). Notice how the posterior urethra is closed off at rest but wide open during urination. The RUG nicely demonstrates the exact length and location and severity of the bulbar stricture, and the VCUG confirms the posterior uretha is normal.

RUG

VCUG
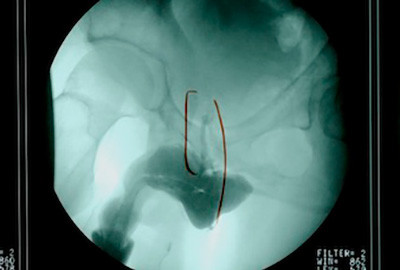
However, if there is a narrowing within the posterior urethra during voiding, then this indicates a stricture. In this example, there is a bulbar stricture seen during injection. The posterior urethra is not wide open as would be expected at rest. However during voiding, the area of the membranous urethra remains very narrow.
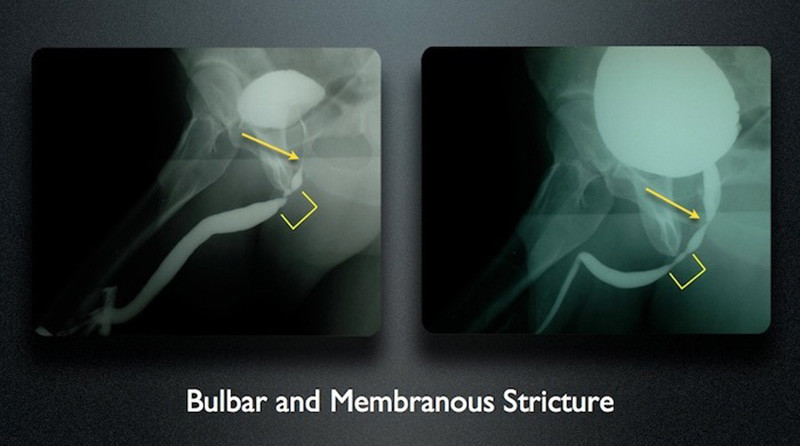
In the above example, if the RUG were the only test performed, then the additional posterior stricture would have been missed. We do not want to risk missing strictures when doing imaging and being “surprised” to find additional strictures at the time of surgery. This could compromise the surgery, and it is for this reason that we perform complete imaging when indicated. Together, the RUG and VCUG provide an evaluation of the entire anterior and posterior urethra. The patient with the 2 separate strictures had a history of dilations and internal stricture incisions, called direct vision internal urethrotomy. Most likely, the stricture was initially only involving the bulbar urethra, and the failed treatments through the penis caused damage to the membranous urethra.
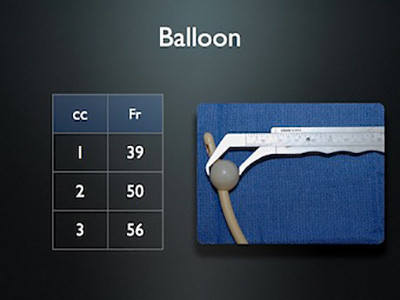
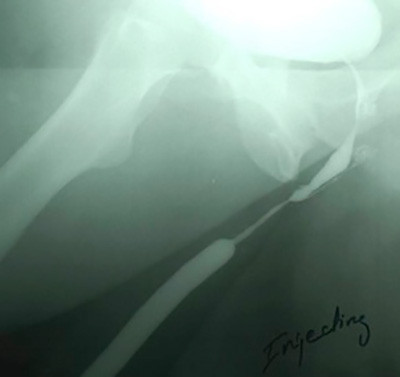
We have actually seen patients referred for strictures in the bulbar urethra (urethral stricture in the part of the urethra under the scrotum far from the tip of the penis) who previously underwent imaging using a balloon technique, and then developed a separate stricture where the catheter was inflated towards the tip of the penis. These patients then require reconstruction of both strictures. After the balloon is inflated, any traction on the catheter to place the penis on stretch can lead to the catheter being pulled out. Therefore, films are often obtained with the penis not on stretch, and the stricture length is underestimated. The following is an example of an outside study using a balloon inflated in the urethra with the penis not on stretch. The impression was that the stricture was 2cm in length. We repeated the study with the penis on stretch using our standard technique, and the stricture was actually 5 cm in length.


We have seen a number of operative dictations from failed surgeries where it was indicated that during the surgery, it was discovered that the stricture length was longer than anticipated. In these cases, proper imaging would have accurately predicted the stricture length and location, allowing the proper procedure to be planned.
For example, when the position is not sufficiently oblique, the urethra is seen “on end”, preventing proper assessment of the stricture length. If someone is showing you a pencil, and the tip of the pencil is facing you and the rest of the rest of the pencil is facing away from you, it is hard to know the length of the pencil. However, if you see the pencil from the side, you can see both ends and everything in between, and you can tell the length. Same with urethral imaging.
This is the example of an outside film that suggested a 2 cm obliteration of the urethra. The patient was flat on the table with the film taken front to back. We repeated the study with the patient in the proper oblique position (turned partially sideways with the penis on stretch to the side, and the actual length of obliteration was 8 cm.
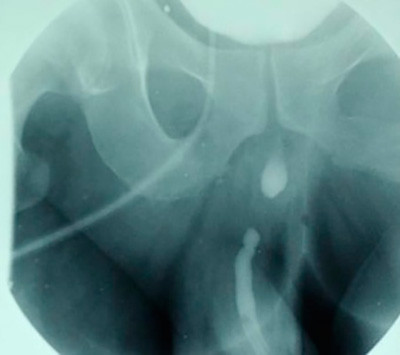

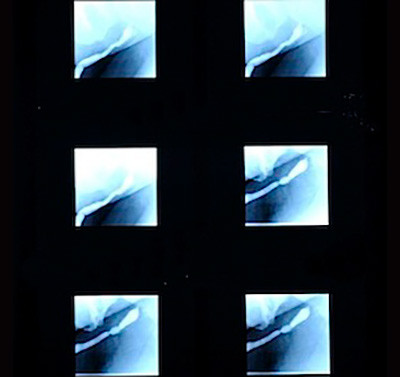
Almost all outside studies we see are performed using fluoroscopy, an imaging technique that allows many films to be taken in a short period of time. This offers the advantage of instant gratification where you can take images in real time, like a movie. The problem with most fluoroscopic studies is that round low quality images are produced with a very small field of view. Often, only a portion of the urethra is seen. We prefer 1 good urethral image over 70 bad images. The following are outside images in comparison to the repeat urethral X-ray imaging performed at our center. Notice how the 1 good image clearly shows the location and length of the area of narrowing.
In some cases, the physicians and technicians attempt to fill the bladder by advancing a catheter into the bladder to instill contrast. However, if a catheter could be easily advanced into the bladder, then that would indicate there is no stricture. Since patients do have urethral strictures, this approach to urethral stricture diagnostic testing generally traumatizes the urethra. This is a fluoroscopic image obtained after an attempt was made by the radiologist to advance a catheter through the stricture to then inject contrast. This caused a urethral tear, and the contrast then leaked into the surrounding tissues. This patient was then referred to our center and the study was repeated without the use of a catheter as shown. There was no need to catheterize or cause damage, and we were able to clearly identify the urethral stricture.

Dr. Gelman strongly believes that it is best that Urologists who perform urethral reconstructive surgery personally perform or at least supervise high quality proper urethral imaging procedures, as accurate maging is necessary to provide a specific diagnosis and formulate a correct treatment plan.